Surgery: Total Knee Replacement (TKR) / Total Knee Arthroplasty (TKA)
✨ Too Long Didn’t Read (TLDR) / Summary
Who needs a Total Knee Replacement? People with symptomatic knee arthritis (pain, stiffness, limited function) confirmed by exam/imaging.
What is a Total Knee Replacement? Surgical resurfacing of the bottom femur, top tibia, and backside of the knee cap (patella bone) to create a smoother, less painful knee joint.
Why it matters: Can reduce pain and improve mobility. Recovery takes effort and patience.
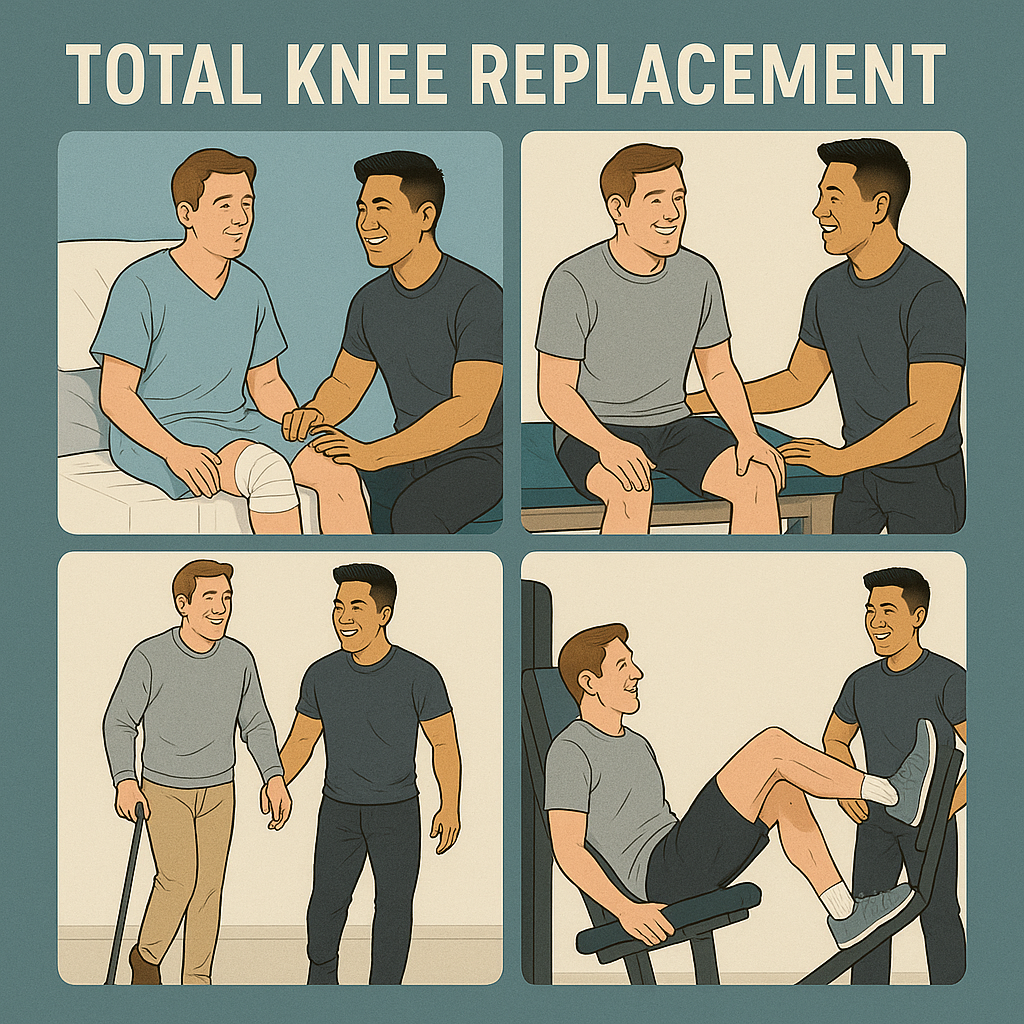
Timeline: Patients can expect gradual improvement after surgery. Physical therapy can last anywhere from 4 to 12 weeks after surgery. Full, functional recovery commonly spans 9–12 months.
Rehab keys: Early movement, home exercise, strength and range-of-motion goals (about 120–125° flexion, 0° extension).
🧾 Condition-Specific General Information
Total knee arthroplasty (TKA), also called total knee replacement (TKR), is a common surgery for knee osteoarthritis when pain and disability persist despite non-surgical care.
Typical candidate: Often age 50 years or older with a symptomatic, painful knee.
How is this diagnosed? Typically diagnosed using an x-ray. Imaging may note “osteoarthritis,” “degenerative joint disease,” or “joint space narrowing/bone-on-bone.”
Common symptoms: Front or side knee pain; pain with walking, climbing or going down stairs, getting in/out of chairs. Symptoms will typically have a gradual onset over time, unless there is trauma involved.
Goal of surgery: Decrease pain, improve function, and quality of life.
Credit: @Dr. Anand Jadhav (@dr.anandjadhav398(YouTube))
💙 For Patients
What to expect: Pain after surgery is normal—it often feels different than your arthritis pain. This pain is often intense so do not be surprised! You’ll likely work with a physical therapist afterwards and do exercises at home.
🏃 Early Movement Helps
Early, safe walking and gentle exercises help prevent stiffness, blood clots (like a deep vein thrombosis (DVT)), and muscle loss. Oftentimes, patients will be up and walking within the same day or next day after their surgery.
It’s safe (and important!) to begin walking early with guidance.
📈 Your Rehab Targets
Range of motion: Aim for about 120–125° knee bend and 0° straightening. Don’t be surprised when you are stiff and cannot fully straighten or bend your knee after surgery - this is normal. You just had a major surgery and your body needs time to heal. Keep working at it, you’ll get there!
Activities:
The goal is always to get back to independent walking without any device helping you. Don’t be surprised when you have to walk with an assistive device like a cane or walker at the start of your recovery. This will get better as you continue to recover!
Driving returns when you’re safe, strong, and off any medications that may impair your ability to drive - this is a great question to ask your surgical team about.
Some patients may have goals that involve more activity like golf, tennis, hiking and more - discuss these with your surgical team and physical therapist to establish a plan!
❓ Smart Questions to ask Your Physical Therapist
How long is recovery and how often should I do home exercises?
How many PT visits will I need and what will sessions look like?
What range of motion should I aim for and why does it matter?
When can I walk unaided, drive, go back to the gym, or run?
How long will swelling and soreness last, and will I need help at home?
Will my knee ever feel “normal” again?
🧾 Common Patient Questions for Surgeons
How can I communicate with the surgical team?
What “red flags” should you look for? (signs of infection or other post-operative concerns)
What is the closure type (stitches vs. glue) and wound care plan? When can I get my incision wet and shower?
What medication will I need? Do I have to stop any of my other medications?
When can I drive? Will I need someone to drive me while I recover?
How long does the swelling last?
Is there anything I will not be able to do after I fully recover from the surgery?
When can I expect to “feel normal” again?
🧊 Managing Pain, Swelling, and Motion
Typically, surgeons will recommend using ice or cryotherapy regularly during the first 4 weeks to help with pain.
Elevation is one of the best ways to manage your swelling - it will be uncomfortable but try to elevate your knee so that your surgical leg is above your heart.
As much as possible, avoid putting anything underneath the knee during the first few weeks when resting - your knee is healing and you want it to heal straight! If it heals in a bent position at rest, it becomes very difficult to get the knee completely straight later on.
Stick with your home exercise plan—consistency beats intensity early on.
👩⚕️ For Providers
Set expectations early and pair objective targets with functional outcomes. Validate fears, use plain language, and check understanding with teach-back.
🔑 Patient Education Priorities
Timeline: Emphasize a 9–12 month recovery arc, with early wins and later refinements.
Pain expectations: Normalize post-op pain quality vs. pre-op arthritis pain. Ensure that you are communicating that this is a major surgery and there will be significant pain afterwards. Give the patient pain management strategies to help!
Home exercise: Explain why, how often, and how it links to function (stairs, gait, transfers, kneeling).
Emphasize the “why” behind the exercises. Example: Quad sets are to help activate the muscles and facilitate end-range knee extension to help you walk.
ROM goals: About 120–125° flexion and 0° extension.
🏥 Rehab Considerations
Early PT supports range of motion, strength, and functional mobility.
Balance & gait training are beneficial through ~9 months post-op.
NMES can aid quadriceps strength and function early and long-term. Keep in mind, quadriceps strength can drop by about 50% right after surgery - NMES can get the patient back to walking comfortably, faster.
Progressive strengthening around 6-8 weeks can help improve strength, ROM, and function—adjust to patient tolerance and precautions.
🤝 Communication Tips (Soft Skills)
Translate targets into daily life: “0° extension helps your knee feel steady when you stand; 120° helps with stairs and tying shoes.”
Use reflective listening: “It sounds like you’re worried about the pain at night—let’s plan for that.”
Close with teach-back: “Just to confirm, how will you use ice and when will you do your home program?”
📂 Supplemental Downloads / Information
📄 Patient Handout: Patient Questions throughout TKA
📄 Patient Handout: TKA Recovery Tips
📄 Provider Checklist: Post-TKA Education Points
📚 APTA Clinical Practice Guideline on TKA (Jette 2020)
📚 Kneeling After TKA (Wallace 2019)
This content drafted, researched, edited, and generated by:
Jackson Kojima, PT, DPT & McKinley Pollock, PT, DPT
Jackson Kojima, PT, DPT, OCS is a physical therapist with an extensive background in orthopedics, geriatrics, and sports rehabilitation. Dr. Kojima is a board-certified orthopedic specialist (OCS) with a passion for post-operative rehabilitation and enjoys treating multi-factorial conditions like low back pain and generalized joint pain. Dr. Kojima earned his doctorate of physical therapy from Campbell University in 2021 and currently lives in Kernersville, NC.
McKinley Pollock, PT, DPT, OCS, CSCS is a physical therapist with a background in orthopedics and sports rehabilitation. Dr. Pollock earned his doctorate of physical therapy from Campbell University in 2021, is a board-certified orthopedic specialist (OCS), and certified strength and conditioning specialist (CSCS) who enjoys combining lessons learned from his DPT training and research, translating these into clinical practice. Dr. Pollock’s passions include promoting relationships between patients & clinicians to promote clinical effectiveness, satisfaction, and efficiency, the implementation of primary preventative medicine into clinical practice, and leadership and education development.
© 2025 The Joint Connection Company. All rights reserved.
The content on this website, including all text, graphics, and materials, is the exclusive property of The Joint Connection Company and is protected by applicable copyright and intellectual property laws. No part of this site may be reproduced, distributed, or used without prior written permission.