The Heart of Healing: Why Empathy Matters on Both Sides of the Exam Table
An illustrated healthcare scene showing a provider and patient sharing a compassionate conversation during a medical exam, reinforcing the theme “The Heart of Healing: Why Empathy Matters on Both Sides of the Exam Table.” The provider stands warmly beside the seated patient, creating a supportive, trust-centered interaction.
✨ Too Long Didn’t Read (TLDR) / Summary
Empathy is the heart of healing. It’s not just kindness—it’s the bridge between medical skill and human understanding.
When clinicians show empathy, patients trust more, share more, and heal better. Studies show empathy improves satisfaction, adherence, and even physical health outcomes.
Patients play a role too. Openness, honesty, and clear communication make care more personal and effective.
Empathy can be taught. Training that focuses on communication, relationship-building, and emotional resilience strengthens both clinicians and patients.
Empathy can fade under stress. Heavy workloads, emotional fatigue, and “professional distancing” can make it hard for providers to stay connected.
The brain rewards connection. Warm communication and trust has been shown to reduce stress, lower blood pressure, and help the body feel safe enough to heal.
Small shifts make a big difference. Simple actions like listening fully, checking for understanding, or expressing appreciation build trust and better outcomes.
Introduction
Empathy isn’t just a “nice-to-have” in healthcare—it’s the bridge that connects medical expertise with human experience. When providers attempt to understand what their patients are going through, care feels personal, not procedural. And when patients sense that their clinicians genuinely care, they’re more likely to trust, follow advice, and feel empowered in their own recovery.
But empathy is complex. It can be emotionally draining, misunderstood, and difficult to sustain in a busy medical world. For both clinicians and patients, learning how to balance empathy with self-care can transform the experience of healthcare itself.
What Empathy Really Means in Healthcare
Empathy is more than feeling sorry for someone—it’s understanding another person’s perspective and responding in a way that shows care and respect. Research shows that empathy has measurable effects on patient satisfaction, adherence, and even physical health outcomes.
To fully understand empathy, you have to understand the different kinds and layers. Cognitive empathy means understanding what someone else is feeling; emotional empathy means sharing those feelings; and empathic concern (or compassion) means caring enough to help. These work together to create a strong clinician–patient bond that supports healing.
Clinicians who express empathy through their tone of voice, facial expressions, and language reduce patient stress and build trust. Patients who feel seen and understood are more likely to share honest information, make lifestyle changes, and follow care plans effectively.
Why Empathy Can Be Hard to Maintain
Despite its benefits, empathy often fades during medical training. Howick et al, 2023 reviewed 16 studies and found that empathy commonly declines as students progress through medical school, often because of heavy workloads, stress, and limited emotional support. Over time, students learn to “distance” themselves as a coping mechanism, which can reduce human connection in care.
In practice, clinicians face additional challenges. Emotional exhaustion, compassion fatigue, and time pressure can make it difficult to stay open and connected. Without the right tools, even the most caring professionals can feel drained or disconnected from the people they serve.
How the Brain Helps Us Stay Connected
Neuroscience provides an interesting perspective on empathy through something called the “free-energy principle.” In simple terms, our brains are prediction machines. They constantly guess what’s going to happen next—what we’ll see, feel, or hear. When our guesses are right, we feel safe and in control. When they’re wrong, we feel surprised or uneasy.
In healthcare, empathy helps bridge those prediction gaps. When a provider offers a calm tone, steady eye contact, and reassurance, it signals safety to the patient’s brain. This reduces stress hormones, lowers blood pressure, and strengthens trust. In this way, empathy doesn’t just feel good—it helps the body heal.
Practical Steps for Clinicians
Begin each visit with a pause. Take a moment to reset before entering the room.
Ask open-ended questions such as, “What’s most important to you today?”
Listen without interrupting for at least 30 seconds. It sounds small but builds trust.
Practice teach-back—ask the patient to explain what they understood to ensure clarity.
Reflect after emotionally intense encounters to prevent burnout.
Empathy can also be taught and reinforced through training. Studies show that structured programs focusing on communication, relationship building, emotional resilience, and counseling skills significantly improve both clinician well-being and patient satisfaction.
The Patient’s Role in Empathy
Empathy is not a one-way street. Patients play an active part, too. By being open about their worries, preferences, and values, patients help providers understand their perspective. When patients feel safe to speak up—especially about fears or confusion—they create space for empathy to grow.
Simple actions, like making eye contact, expressing appreciation, or asking clarifying questions, build connection. A strong partnership between patients and providers turns medical visits into meaningful conversations, not rushed transactions.
Practical Steps for Patients
Prepare questions before your appointment.
Share how you’re feeling, not just your symptoms.
Be honest about what’s working or not working in your care plan.
Express appreciation—your provider is human, too.
Remember: asking for clarity isn’t “bothering” your clinician—it’s part of good care.
Empathy as a Shared Responsibility
Empathy should not be an added burden; it should be part of how we deliver and receive care. Effective communication means respecting patients as people—not just diagnoses—and using language that shows care and awareness.
When clinicians and patients work together to understand one another, healthcare becomes more humane, more effective, and more fulfilling. Empathy connects us—not only to better outcomes but also to each other.
At The Joint Connection Company, we believe that connection is treatment. By nurturing empathy on both sides of the exam table, we can all help make healthcare feel a little more human again.
References
Nembhard IM, David G, Ezzeddine I, Betts D, Radin J. A systematic review of research on empathy in health care. Health Serv Res. 2023;58(2):250-263. doi:10.1111/1475-6773.14016
Keshtkar L, Madigan CD, Ward A, et al. The Effect of Practitioner Empathy on Patient Satisfaction: A Systematic Review of Randomized Trials. Ann Intern Med. 2024;177(2):196-209. doi:10.7326/M23-2168
Hojat M, DeSantis J, Shannon SC, Mortensen LH, Speicher MR, Bragan L, LaNoue M, Calabrese LH. The Jefferson Scale of Empathy: A nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23(5):899-920. doi:10.1007/s10459-018-9839-9
Decety J. Empathy in Medicine: What It Is, and How Much We Really Need It. Am J Med. 2020;133(5):561-566. doi:10.1016/j.amjmed.2019.12.012
Geyer C. Empathy and Language in the Clinician Patient Relationship: Improving the Translation of Evidence to Practice. Am J Health Promot. 2021;35(4):590-592. doi:10.1177/08901171211002328
Howick J, Dudko M, Feng SN, et al. Why might medical student empathy change throughout medical school? a systematic review and thematic synthesis of qualitative studies. BMC Med Educ. 2023;23(1):270. doi:10.1186/s12909-023-04165-9
Lajante M, Del Prete M, Sasseville B, Rouleau G, Gagnon MP, Pelletier N. Empathy training for service employees: A mixed-methods systematic review. PLoS One. 2023;18(8):e0289793. doi:10.1371/journal.pone.0289793
This content drafted, researched, edited, and generated by:
McKinley Pollock, PT, DPT
McKinley Pollock, PT, DPT, OCS, CSCS is a physical therapist with a background in orthopedics and sports rehabilitation. Dr. Pollock earned his doctorate of physical therapy from Campbell University in 2021, is a board-certified orthopedic clinical specialist (OCS), and certified strength and conditioning specialist (CSCS). Dr. Pollock enjoys combining lessons learned from his DPT training and research, translating these into clinical practice. His passions include promoting relationships between patients & clinicians to promote clinical effectiveness, satisfaction, and efficiency, the implementation of primary preventative medicine into clinical practice, and leadership and education development.
Surgery: Rotator Cuff Repair
✨ Too Long Didn’t Read (TLDR) / Summary
Who needs a Rotator Cuff Repair? People with shoulder pain, weakness, or limited movement from a torn rotator cuff tendon (from trauma, overuse, or age‑related changes).
What is a Rotator Cuff Repair? Surgical repair of one or more of the four rotator cuff tendons that stabilize and move the shoulder. As a patient, you have a choice and opportunity to talk with your physician about options - whether to manage the tear with or without surgery.
Note: Not all rotator cuff tears necessarily need repairing - in fact, it’s not uncommon for people with small-to-medium sized rotator cuff tears to recover and get back to their normal, every day function without surgery!
Why this matters: If deemed necessary, rotator cuff repairs can reduce pain, improve strength, and restore function.
Post-operative timeline: Typically, patients will be in a sling for 4–6 weeks. Gradual progression towards day-to-day activities will occur 2-4 months post-operatively. Sports/heavy work will begin and resume ~6 - 12 months post-operatively.
Note: This timeline depends on the severity of the tear, the muscle torn, and the repair technique/surgeon’s preferences. Small tears will heal quicker ; large tears will heal slower. Talk with your surgeon and physical therapist to tailor this plan specifically to you!
Patient keys: Talk with your surgeon and physical therapist to determine best course of action. Keep log of small wins to track progress and remain encouraged throughout a long rehabilitation. Perform home exercise program consistently and be patient with yourself.
Rehab keys: Protect healing tissue early → restore shoulder motion → strengthen cuff, deltoid, and scapular muscles to provide stability.
🧾 Condition-Specific General Information
The rotator cuff is a team of four small muscles and tendons that keep the shoulder joint stable and let you lift, rotate, and reach. Tears can happen from a fall, heavy lifting, repetitive overhead work, or age‑related tendon wear. Not everyone notices pain right away—some feel weakness or limited motion first. People with rotator cuff tears can feel pain when they lift their arm overhead, reach, lift heavy objects, and more.
Treatment options include conservative care (AKA: non-operative care) and surgery:
Conservative: Physical therapy to reduce pain, restore motion, and strengthen the shoulder using the muscles that remain intact.
Surgical: Repair of torn tendon(s) when pain or function doesn’t improve with therapy or when the tear is significant.
Diagnostic & Management Considerations
Imaging is not always needed, as in-clinic testing can help rule in/out rotator cuff tear ; tears can be confirmed using MRI or ultrasound when indicated.
NSAIDs, acetaminophen, and injections may help reduce short-term pain.
Need to talk to your physician for guidance
Surgery remains most-appropriate for selected full-thickness tears.
Need to talk to your surgeon for guidance
Video Credit: Demystifying Science (link: https://www.youtube.com/watch?v=Dwuxqs_h3Js)
💙 For Patients
❓ Smart Questions for Your Healthcare Team
Do you feel that I need surgery? Are there other options other than surgery?
Are there any exercises I can do to help my pain or mobility?
How long is the recovery?
What can I NOT do after surgery?
What can I safely do after surgery?
When can I drive?
Will I have pain afterward? How will this be managed?
How long does a repair last?
Can I re-injure my shoulder? What activities do I have to avoid?
Will I be able to get back to all of my activities?
Tip: Pick 2-3 activities that you want others to ask about specifically
What happens if I don’t have surgery?
Can I wait to schedule surgery?
Your Healing Timeline: What to Expect
Recovery from a rotator cuff repair is significant—it deserves patience and support.
0–6 Weeks After Surgery: Protection Comes First
Expect to wear a sling for 4–6 weeks to protect the repair.
You will generally not use your arm during this time.
Your physical therapist will focus on gentle passive range of motion—they move your arm for you.
6–12 Weeks: Gradual Movement Returns
Depending on what was repaired, you may not start moving your arm on your own for 2–3 months.
You may begin assisted movement and eventually active motion as the tissue heals.
3–6 Months: Strength & Function
Most patients return to normal daily activities and begin restoring strength by 6 months.
Returning to sports, heavy lifting, or overhead work can take 6–12+ months.
Full Recovery Expectations
Rotator cuff healing can continue for up to one year, especially for patients returning to demanding activities.
📈 Your Rehab Targets
Protect first: Respect sling and movement restrictions.
Regain motion gradually: Directed by your physical therapist guidance and surgeon’s protocol.
Strengthen: Rotator cuff, deltoid, and scapular stabilizers to ensure muscles work together to produce motion.
Return step-by-step: Lifting, work tasks, and sports will be reintroduced safely.
🧊 Managing Pain & Daily Life
In the first 4–6 weeks
Use ice/cryotherapy to help with swelling and pain.
Keep the sling on unless your team says otherwise.
Avoid using the surgical arm for lifting/reaching.
Tip: Wearing the sling will help you avoid accidentally using your surgical shoulder
Consistency beats intensity
Follow your home exercise plan as prescribed.
Share pain/sleep issues with your therapist and surgeon.
Keep a log of small wins to track your progress and keep your spirits high
Celebrate small wins to stay motivated.
👩⚕️ For Providers
🔑 Patient Education Priorities
Timeline: Sling 4–6 wks; functional recovery 4 – 12 months (depending on size of tear and repair procedure); set realistic milestones.
Pain expectations: Normalize repair pain vs. pre‑op symptoms; discuss pain strategies, particularly at night.
Rehab progression: PROM → AAROM → AROM → strengthening → functional return.
Expectation setting: Full recovery may take up to a year depending on goals.
Essential Tip: Celebrate small wins and milestones!
🤝 Communication Tips (Soft Skills)
Translate goals → daily life: “Strengthening these muscles helps you reach overhead to put away dishes.”
Reflective listening: “It sounds like you’re worried about reinjury—let’s review how the sling protects your shoulder and how we’ll progress safely.”
Teach‑back: “Just so I’m clear, how will you protect your shoulder during the first 6 weeks?”
🧾 Common Patient Questions (from anecdotal experience)
Do you think I need surgery? How do I know if I need surgery?
When will I be able to drive?
When can I come out of the sling?
What are strategies to help me sleep better? Do I have to sleep in my sling?
How can I manage my pain?
I shrug my shoulder when I lift my arm - what can I do about this?
When do my lifting restrictions come off?
How long does the repair last?
Could I need surgery again?
What happens if I wait to have surgery?
Will my shoulder ever feel “normal” again?
🏥 Rehab Considerations & Clinical Pearls ⚪️
Restore ROM early without compromising healing
Address posterior capsule and pectoralis minor tightness
Strengthen the rotator cuff and scapular stabilizers (including serratus anterior, upper trap, and lower trap) to establish upward rotation scapular biomechanics
Gradual, tested, graded progression will give comfort to both you as a clinician and the patient - have objective information to track progress!
Integrate task-specific and return-to-work planning
Initiate progressive strengthening ~12 wks, tailored to tear size and tissue quality.
Advance to functional tasks: lifting, overhead reach, sport‑specific progressions.
📂 Supplemental Downloads / Information
📄 Patient Handout: Common Questions for Before and After Rotator Cuff Repair Surgery
📄 Provider Checklist: RTC Education Points Before & After Surgery
📚 Example: Rotator Cuff Repair Physical Therapy Protocol (Credit: Massachusetts General Hospital)
📚 Example: Massive Rotator Cuff Repair Physical Therapy Protocol (Credit: Ohio State College of Medicine)
Bibliography / Citations:
American Academy of Orthopaedic Surgeons. Management of Rotator Cuff Injuries Evidence-Based Clinical Practice Guideline. Published August 18, 2025. https://www.aaos.org/rccpg2025
American Academy of Orthopaedic Surgeons. Management of Rotator Cuff Injuries Evidence-Based Clinical Practice Guideline. https://www.orthoguidelines.org/guideline-detail?id=1869&tab=all_guidelines
American Academy of Orthopaedic Surgeons. Management of Rotator Cuff Injuries Evidence-Based Clinical Practice Guideline. https://www.orthoguidelines.org/guideline-detail?id=1870&tab=all_guidelines
American Academy of Orthopaedic Surgeons. Management of Rotator Cuff Injuries Evidence-Based Clinical Practice Guideline. https://www.orthoguidelines.org/guideline-detail?id=1891&tab=all_guidelines
Lafrance S, Charron M, Roy JS, et al. Diagnosing, Managing, and Supporting Return to Work of Adults With Rotator Cuff Disorders: A Clinical Practice Guideline. J Orthop Sports Phys Ther. 2022;52(10):647-664. doi:10.2519/jospt.2022.11306
Hodakowski AJ, McCormick JR, Damodar D, et al. Rotator cuff repair: what questions are patients asking online and where are they getting their answers? Clin Shoulder Elbow. 2023;26(1):25.
Dickinson RN, Ayers GD, Archer KR, et al. Physical therapy versus natural history in outcomes of rotator cuff tears: the ROW cohort study. J Shoulder Elbow Surg. 2019;28(5):833-838. doi:10.1016/j.jse.2018.10.001
Dickinson RN, Kuhn JE. Nonoperative Treatment of Rotator Cuff Tears. Phys Med Rehabil Clin N Am. 2023;34(2):335-355. doi:10.1016/j.pmr.2022.12.002
This content drafted, researched, edited, and generated by:
Jackson Kojima, PT, DPT & McKinley Pollock, PT, DPT
Jackson Kojima, PT, DPT, OCS is a physical therapist with an extensive background in orthopedics, geriatrics, and sports rehabilitation. Dr. Kojima is a board-certified orthopedic clinical specialist (OCS) with a passion for post-operative rehabilitation and enjoys treating multi-factorial conditions like low back pain and generalized joint pain. Dr. Kojima earned his doctorate of physical therapy from Campbell University in 2021 and currently lives in Kernersville, NC.
McKinley Pollock, PT, DPT, OCS, CSCS is a physical therapist with a background in orthopedics and sports rehabilitation. Dr. Pollock earned his doctorate of physical therapy from Campbell University in 2021, is a board-certified orthopedic clinical specialist (OCS), and certified strength and conditioning specialist (CSCS). Dr. Pollock enjoys combining lessons learned from his DPT training and research, translating these into clinical practice. His passions include promoting relationships between patients & clinicians to promote clinical effectiveness, satisfaction, and efficiency, the implementation of primary preventative medicine into clinical practice, and leadership and education development.
Get More From Every Minute: How to Make Short Appointments Count
✨ Too Long Didn’t Read (TLDR) / Summary
Healthcare visits are shorter than ever — and that can feel frustrating for everyone involved. But with a little preparation and the right communication habits, those 15 minutes can become powerful, productive, and personal.
Patients: Come in prepared with your top concerns, organized info, and clear questions.
Providers: Use structure, empathy, and small cues to help patients feel heard — even on a tight schedule.
When both sides work together, time becomes less of an obstacle and more of a tool for better care.
Introduction
Let’s be honest: nobody likes feeling rushed in a doctor’s office. Patients spend days waiting for an appointment that sometimes lasts less time than their morning coffee break. Providers juggle packed schedules, endless charts, and the constant tick of the clock.
And yet — every once in a while — there’s that great visit: the one where everything clicks. You leave feeling understood, reassured, and like your health is in good hands.
What’s the secret? It’s not luck. It’s communication and preparation — on both sides of the exam table.
This post explores how patients and providers can turn short visits into meaningful ones that deliver clarity, trust, and next steps — without anyone feeling like they’re in a speed-dating session for healthcare.
🧾 For Patients: How to Prepare for Short Appointments
1. 🎯 Know Your Top Three
Before you even set foot in the office, decide your top three concerns for the visit. Write them down — yes, on paper or in your phone. This keeps your appointment focused and helps you leave feeling like your main needs were addressed.
Example: “1. My new chest tightness, 2. Refill on my blood pressure meds, 3. Questions about side effects.”
If something else comes up, that’s okay — but start with the most important issues first.
2. 💊 Bring the Evidence
No, not like a crime show — but your medication list, supplements, and any recent test results are gold.
Even better: take photos of the labels or bottles with your phone. It’s fast, accurate, and saves your clinician from deciphering handwriting that looks like a secret code.
3. 📝 Ask for a Recap
After your visit, politely ask:
“Could I get a printed or emailed summary?”
Most offices can do this easily. It helps you remember what was said, when to follow up, and how to take your medications. (Bonus: it prevents the “Wait, what did my doctor say?” moment two days later.)
4. ⏰ Arrive Early and Breathe
Running late means less face time. Arrive 10–15 minutes early so you can relax, fill out paperwork, and mentally focus. You’ll feel calmer — and calm brains listen and retain information better.
5. ❤️ Be Honest, Not Heroic
If something feels off, say so. You don’t have to tough it out or minimize symptoms. Clinicians want your real experience, not your “everything’s fine” face.
🩺 For Providers: How to Maximize Empathy and Efficiency
1. 🚪 Start Before You Enter
Before walking into the room, take one deep breath and set your intention:
“I have 15 minutes to make this person feel heard.”
That small mental pause can transform tone, body language, and focus.
2. 🙋♂️ Open with the Patient’s Agenda
Begin with:
“What’s most important for us to cover today?”
It’s a simple question, but it tells the patient, “This is your time.” Then, together, you can triage priorities and make sure the visit feels purposeful.
3. 🧩 Use “Micro-Empathy”
Even brief interactions can be warm and personal.
Make eye contact when you greet.
Nod as patients speak.
Reflect what you heard: “It sounds like your headaches have been getting worse.”
Tiny cues of understanding go a long way — and take seconds.
4. 💬 Teach-Back Saves Time Later
End with something like:
“Can you tell me in your own words what the plan is, just so I know I explained it clearly?”
It’s a gentle check that prevents confusion, follow-up calls, and mistakes — a win-win for both parties.
5. 🧠 Document Strategically
Typing while talking can feel robotic. If possible, make eye contact during key moments, then finish notes afterward. Even narrating your process (“I’m just adding that to your chart”) keeps patients engaged rather than feeling ignored.
💡 Conclusion
A short visit doesn’t have to mean a shallow one. When patients come prepared and providers stay present, those few minutes can deliver clarity, comfort, and connection.
Efficiency and empathy aren’t opposites — they’re teammates. The best care happens when both sides speak the same language: one of respect, curiosity, and understanding.
So whether you’re wearing the white coat or the hospital gown, remember — a little prep and a little heart go a long way.
📎 Supplemental, Downloadable Content
🧾 Downloadable “Prep Sheet” for Patients
Oh hi - thank you for reading! We hope you enjoyed and that you are able to take these tools with you to get the most out of your next healthcare appointment! Below are some “bloopers” that ChatGPT gave us when trying to have a caption for this blog post… They were too good not to share!
This content drafted, researched, edited, and generated by: McKinley Pollock, PT, DPT
McKinley Pollock, PT, DPT, OCS, CSCS is a physical therapist with a background in orthopedics and sports rehabilitation. Dr. Pollock earned his doctorate of physical therapy from Campbell University in 2021, is a board-certified orthopedic specialist (OCS), and certified strength and conditioning specialist (CSCS) who enjoys combining lessons learned from his DPT training and research, translating these into clinical practice. Dr. Pollock’s passions include promoting relationships between patients & clinicians to promote clinical effectiveness, satisfaction, and efficiency, the implementation of primary preventative medicine into clinical practice, and leadership and education development.
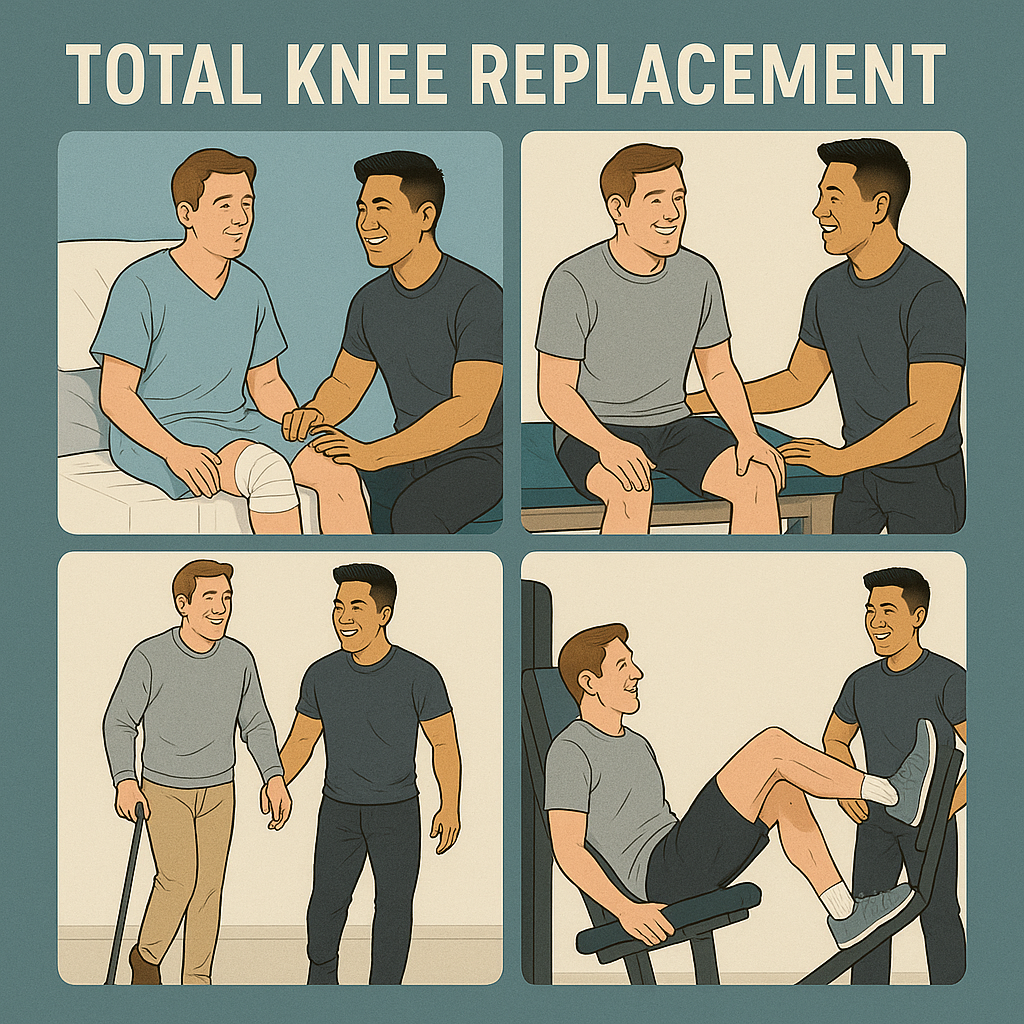
Surgery: Total Knee Replacement (TKR) / Total Knee Arthroplasty (TKA)
✨ Too Long Didn’t Read (TLDR) / Summary
Who needs a Total Knee Replacement? People with symptomatic knee arthritis (pain, stiffness, limited function) confirmed by exam/imaging.
What is a Total Knee Replacement? Surgical resurfacing of the bottom femur, top tibia, and backside of the knee cap (patella bone) to create a smoother, less painful knee joint.
Why it matters: Can reduce pain and improve mobility. Recovery takes effort and patience.
Timeline: Patients can expect gradual improvement after surgery. Physical therapy can last anywhere from 4 to 12 weeks after surgery. Full, functional recovery commonly spans 9–12 months.
Rehab keys: Early movement, home exercise, strength and range-of-motion goals (about 120–125° flexion, 0° extension).
🧾 Condition-Specific General Information
Total knee arthroplasty (TKA), also called total knee replacement (TKR), is a common surgery for knee osteoarthritis when pain and disability persist despite non-surgical care.
Typical candidate: Often age 50 years or older with a symptomatic, painful knee.
How is this diagnosed? Typically diagnosed using an x-ray. Imaging may note “osteoarthritis,” “degenerative joint disease,” or “joint space narrowing/bone-on-bone.”
Common symptoms: Front or side knee pain; pain with walking, climbing or going down stairs, getting in/out of chairs. Symptoms will typically have a gradual onset over time, unless there is trauma involved.
Goal of surgery: Decrease pain, improve function, and quality of life.
Credit: @Dr. Anand Jadhav (@dr.anandjadhav398(YouTube))
💙 For Patients
What to expect: Pain after surgery is normal—it often feels different than your arthritis pain. This pain is often intense so do not be surprised! You’ll likely work with a physical therapist afterwards and do exercises at home.
🏃 Early Movement Helps
Early, safe walking and gentle exercises help prevent stiffness, blood clots (like a deep vein thrombosis (DVT)), and muscle loss. Oftentimes, patients will be up and walking within the same day or next day after their surgery.
It’s safe (and important!) to begin walking early with guidance.
📈 Your Rehab Targets
Range of motion: Aim for about 120–125° knee bend and 0° straightening. Don’t be surprised when you are stiff and cannot fully straighten or bend your knee after surgery - this is normal. You just had a major surgery and your body needs time to heal. Keep working at it, you’ll get there!
Activities:
The goal is always to get back to independent walking without any device helping you. Don’t be surprised when you have to walk with an assistive device like a cane or walker at the start of your recovery. This will get better as you continue to recover!
Driving returns when you’re safe, strong, and off any medications that may impair your ability to drive - this is a great question to ask your surgical team about.
Some patients may have goals that involve more activity like golf, tennis, hiking and more - discuss these with your surgical team and physical therapist to establish a plan!
❓ Smart Questions to ask Your Physical Therapist
How long is recovery and how often should I do home exercises?
How many PT visits will I need and what will sessions look like?
What range of motion should I aim for and why does it matter?
When can I walk unaided, drive, go back to the gym, or run?
How long will swelling and soreness last, and will I need help at home?
Will my knee ever feel “normal” again?
🧾 Common Patient Questions for Surgeons
How can I communicate with the surgical team?
What “red flags” should you look for? (signs of infection or other post-operative concerns)
What is the closure type (stitches vs. glue) and wound care plan? When can I get my incision wet and shower?
What medication will I need? Do I have to stop any of my other medications?
When can I drive? Will I need someone to drive me while I recover?
How long does the swelling last?
Is there anything I will not be able to do after I fully recover from the surgery?
When can I expect to “feel normal” again?
🧊 Managing Pain, Swelling, and Motion
Typically, surgeons will recommend using ice or cryotherapy regularly during the first 4 weeks to help with pain.
Elevation is one of the best ways to manage your swelling - it will be uncomfortable but try to elevate your knee so that your surgical leg is above your heart.
As much as possible, avoid putting anything underneath the knee during the first few weeks when resting - your knee is healing and you want it to heal straight! If it heals in a bent position at rest, it becomes very difficult to get the knee completely straight later on.
Stick with your home exercise plan—consistency beats intensity early on.
👩⚕️ For Providers
Set expectations early and pair objective targets with functional outcomes. Validate fears, use plain language, and check understanding with teach-back.
🔑 Patient Education Priorities
Timeline: Emphasize a 9–12 month recovery arc, with early wins and later refinements.
Pain expectations: Normalize post-op pain quality vs. pre-op arthritis pain. Ensure that you are communicating that this is a major surgery and there will be significant pain afterwards. Give the patient pain management strategies to help!
Home exercise: Explain why, how often, and how it links to function (stairs, gait, transfers, kneeling).
Emphasize the “why” behind the exercises. Example: Quad sets are to help activate the muscles and facilitate end-range knee extension to help you walk.
ROM goals: About 120–125° flexion and 0° extension.
🏥 Rehab Considerations
Early PT supports range of motion, strength, and functional mobility.
Balance & gait training are beneficial through ~9 months post-op.
NMES can aid quadriceps strength and function early and long-term. Keep in mind, quadriceps strength can drop by about 50% right after surgery - NMES can get the patient back to walking comfortably, faster.
Progressive strengthening around 6-8 weeks can help improve strength, ROM, and function—adjust to patient tolerance and precautions.
🤝 Communication Tips (Soft Skills)
Translate targets into daily life: “0° extension helps your knee feel steady when you stand; 120° helps with stairs and tying shoes.”
Use reflective listening: “It sounds like you’re worried about the pain at night—let’s plan for that.”
Close with teach-back: “Just to confirm, how will you use ice and when will you do your home program?”
📂 Supplemental Downloads / Information
📄 Patient Handout: Patient Questions throughout TKA
📄 Patient Handout: TKA Recovery Tips
📄 Provider Checklist: Post-TKA Education Points
📚 APTA Clinical Practice Guideline on TKA (Jette 2020)
📚 Kneeling After TKA (Wallace 2019)
This content drafted, researched, edited, and generated by:
Jackson Kojima, PT, DPT & McKinley Pollock, PT, DPT
Jackson Kojima, PT, DPT, OCS is a physical therapist with an extensive background in orthopedics, geriatrics, and sports rehabilitation. Dr. Kojima is a board-certified orthopedic specialist (OCS) with a passion for post-operative rehabilitation and enjoys treating multi-factorial conditions like low back pain and generalized joint pain. Dr. Kojima earned his doctorate of physical therapy from Campbell University in 2021 and currently lives in Kernersville, NC.
McKinley Pollock, PT, DPT, OCS, CSCS is a physical therapist with a background in orthopedics and sports rehabilitation. Dr. Pollock earned his doctorate of physical therapy from Campbell University in 2021, is a board-certified orthopedic specialist (OCS), and certified strength and conditioning specialist (CSCS) who enjoys combining lessons learned from his DPT training and research, translating these into clinical practice. Dr. Pollock’s passions include promoting relationships between patients & clinicians to promote clinical effectiveness, satisfaction, and efficiency, the implementation of primary preventative medicine into clinical practice, and leadership and education development.
© 2025 The Joint Connection Company. All rights reserved.
The content on this website, including all text, graphics, and materials, is the exclusive property of The Joint Connection Company and is protected by applicable copyright and intellectual property laws. No part of this site may be reproduced, distributed, or used without prior written permission.