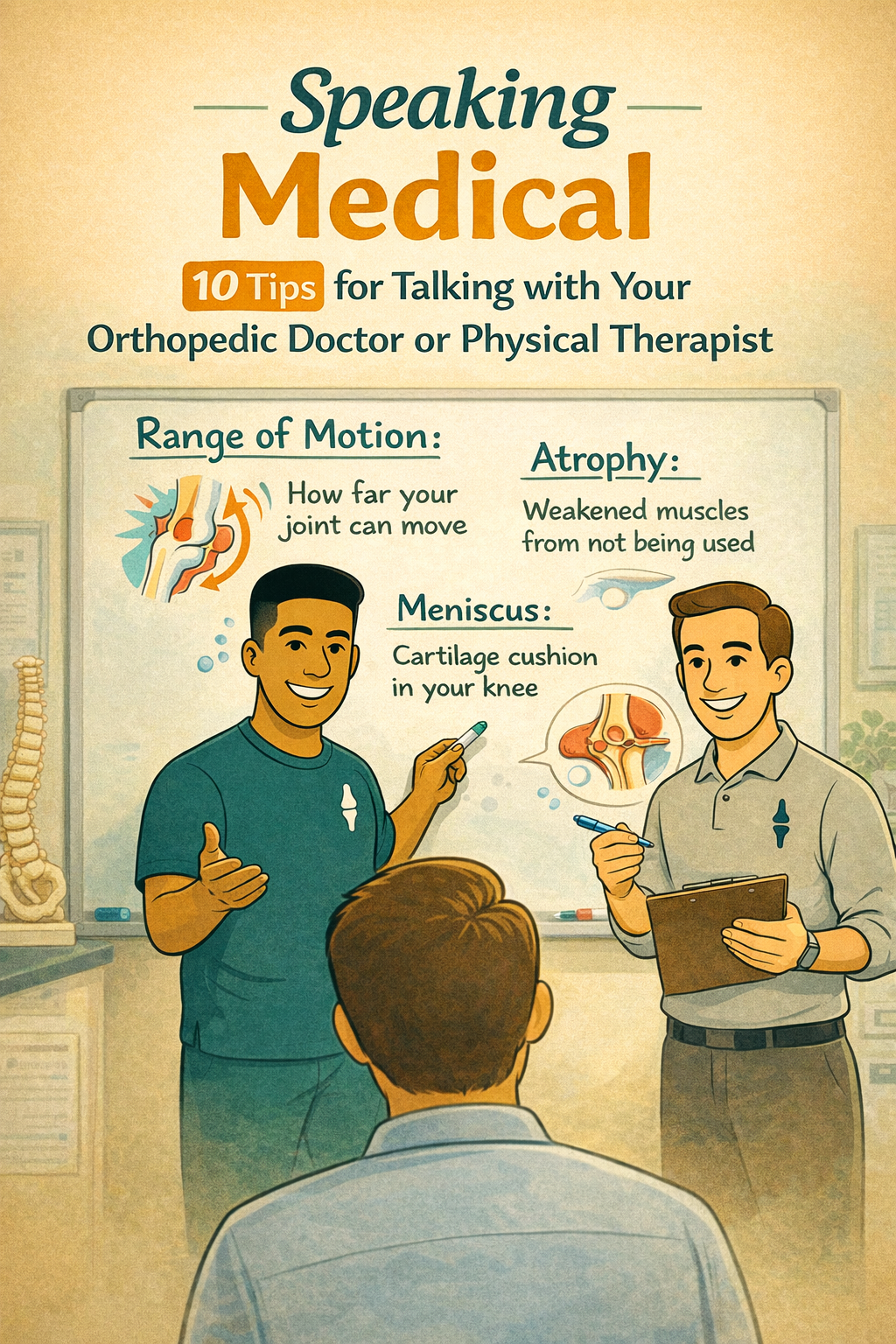
Speaking Medical: 10 Tips for Talking with Your Orthopedic Doctor or Physical Therapist
Walking into a doctor’s office can sometimes feel like stepping into a different country where everyone speaks a language you don’t know. Orthopedic physicians (bone and joint doctors) and physical therapists often use words that sound like a secret code: “range of motion,” “meniscus,” “atrophy.”
But here’s the good news: you don’t need to learn a whole new language to have a good conversation with your healthcare team. You just need a few simple tricks to make sure you understand them—and they understand you.
Here are 10 easy tips to help you “speak medical” during your appointment.
1. Don’t Be Afraid to Say, “I Don’t Understand”
Doctors and therapists sometimes forget that not everyone went to medical school. If something sounds confusing, speak up. Saying, “Could you explain that in everyday language?” is perfectly fine.
2. Learn a Few Common Words
A handful of terms come up a lot:
Range of motion = how far your joint can move
Inflammation = swelling, redness, or heat in your body when something is irritated or injured
Atrophy = muscles loosing their “bulk” or getting weaker because they’re not being used
3. Use Body Maps (Pointing Works!)
You don’t need fancy words to explain pain. Point to the exact spot and say:
“It hurts here when I bend.”
“It feels sharp in this area.”
Your finger is sometimes better than any word.
4. Describe Pain Like You’d Tell a Friend
Pain isn’t just “bad” or “good.” Try using words like:
Sharp
Dull
Throbbing
Burning
Stiff
5. Be Specific With What You're Asking
There are only so many minutes in your appointment. Even if you have pain in your back, knee, shoulder, and toes, try to prioritize which ones you want the doctor to focus on. Feel free to mention any other problems you may have but we recommend choosing one or two issues to focus on. Otherwise, the doctor might not be able to do a full examination and you may risk missing something important.
DO: "My knee really hurts when I run or go up stairs. My head and right shoulder hurt too but my knee is bothering me the most so I really want to focus on my knee today."
DON'T: "My knee really hurts when I run or go up stairs. Also, I get headaches. My right shoulder has also been hurting recently but I'm not sure why. Also, I sprained my ankle when I was 15 and it hasn't been hurting but can you take a look at it?"
6. Ask About Next Steps, Not Just the Problem
It’s easy to get caught up in the diagnosis, but what you really want to know is: What do I do next? Ask things like:
“What can I do at home to help?”
“What should I avoid?”
“What’s the goal of treatment?”
7. Take Notes or Use Your Phone
Appointments go fast. Bring a small notebook, or ask if you can record the conversation on your phone (with permission). This way, you don’t forget the important details when you get home.
8. Repeat It Back in Your Own Words
This is called a teach-back. For example:
Doctor: “You’ll need to ice your ankle for 20 minutes, three times a day.”
You: “So I should ice it morning, afternoon, and evening for 20 minutes?”
This clears up misunderstandings before you leave the office.
9. Bring a Friend if You Need Backup
Having a second set of ears can help. A friend or family member can remind you of questions, or help remember what was said.
10. Remember: You’re Part of the Team
Your doctor or therapist isn’t the boss of your body—you are. They’re the guide, and you’re the driver. Don’t be shy about asking questions, sharing concerns, or saying if something doesn’t work for you.
Final Thoughts
You don’t need a medical degree to have a great conversation with your orthopedic physician or physical therapist. A little preparation, a few simple words, and the confidence to ask questions go a long way.
At the end of the day, “speaking medical” isn’t about memorizing Latin—it’s about making sure you and your healthcare team are on the same page so you can heal, move better, and get back to the life you love.
This content drafted, researched, edited, and generated by:
McKinley Pollock, PT, DPT
McKinley Pollock, PT, DPT, OCS, CSCS is a physical therapist with a background in orthopedics and sports rehabilitation. Dr. Pollock earned his doctorate of physical therapy from Campbell University in 2021, is a board-certified orthopedic clinical specialist (OCS), and certified strength and conditioning specialist (CSCS). Dr. Pollock enjoys combining lessons learned from his DPT training and research, translating these into clinical practice. His passions include promoting relationships between patients & clinicians to promote clinical effectiveness, satisfaction, and efficiency, the implementation of primary preventative medicine into clinical practice, and leadership and education development.